Improving Drug Development and Glioblastoma Xenograft Models
Overcoming Glioblastoma Multiforme (GBM) Drug Development Challenges With Glioblastoma Xenograft Models
Primary brain tumors are highly heterogeneous tumors that cause significant morbidity and mortality. An estimated 700,000 Americans are living with a primary brain tumor — approximately 29% of which are malignant.1 Glioblastoma multiforme (GBM), a grade IV astrocytoma, is the most common malignant brain tumor making up nearly half of these cases (49.1%).1 GBM is also the most devastating malignant brain tumor — the median overall survival is just eight months, and only 6.8% of patients survive five years past diagnosis.2 The current standard of care, which is surgical resection, followed by radiation therapy and temozolomide, and temozolomide maintenance therapy, is largely ineffective, with 95% of patients suffering a relapse.3,4
Bevacizumab can be used for recurrent GBM, yet its use has not improved overall survival, only surrogate outcomes, such as progression-free survival.3,4 Taken together, there is a large unmet need for safe and efficacious therapeutics for GBM.
A Lack of Accurate GBM Preclinical Models is Slowing Development of Effective GBM Therapeutics
A major bottleneck in GBM drug development is a lack of preclinical models that accurately predict pathogenesis and resistance. In a perfect world, GBM models would effectively mimic the:
- Genetic background of the human tumor5
- Intra-tumoral heterogeneity5
- Tumor microenvironment and blood-brain barrier (BBB)5
As with any model, reproducibility and cost-effectiveness are important, yet precisely duplicating optimal preclinical models is particularly challenging for GBM drug developers.
.jpeg?width=600&name=Image%202%20(1).jpeg)
Let’s take a closer look at why.
An Evolving Genetic Background
GBM can be classified at the genetic level as isocitrate dehydrogenase (IDH) - wildtype (WT), which tends to have a worse prognosis than the other category IDH-mutant.6 At the transcriptional level, there are four subtypes, depending on the mutational status and expression level of a handful of genes, including PDGFR, IDH1, EGFR, and NF1.3,4,6 These subtypes are identified using bulk analysis of 200 tumors and highlight the inter-tumoral heterogeneity of GBM.6 Despite this initial characterization, additional mutations in common oncogenic pathways, including CDKN2A/B, TP53, and PTEN, occur within these subtypes, and the genetic landscape of a GBM tumor is constantly changing over time.4,8 Addressing the ever-evolving genetic landscape of an individual tumor and accounting for the extreme genetic variability across individual patients with a traditional pre-clinical model can be like trying to hit hundreds of moving targets, all at once.
Temporal and Spatial Intra-Tumoral Heterogeneity
More recently, single-cell RNA-seq analysis of five GBM tumors has revealed the extreme intra-tumoral heterogeneity within single GBM tumors.8 The study, by Patel et al. shows that GBM tumors can contain representative cells from each transcriptional subtype, which can play a significant role in treatment resistance. Patients whose tumors were classified as being in the pro-neural subtype (which was thought to be the prognostic indicator with the best clinical outcomes) with markers of other subtypes had poorer survival.8,9
The study by Patel et al. also identifies a spectrum of stemness within GBM tumors, likely driven by the presence of glioblastoma stem-like cells (GSCs).4,9 It is now widely accepted that GSCs exhibit a unique tumor-initiating ability, and aggressive GBM tumors, as well as treatment resistance and relapse, are driven by these cell types.4,9 The extreme heterogeneity has been confirmed by additional single-cell genomics studies.8 In addition, studies by Sorttoriva et al., using fluorescence-guided multiple sampling techniques during GBM resection demonstrate the extensive 3D spatial heterogeneity within GBM tumors and confirm that within the same tumor, different subtypes exist.6
The Tumor Microenvironment and the Blood-Brain Barrier
The genetic and transcriptomic complexity and heterogeneity of GBM tumors are further compounded when looking at the immune cells that make up the microenvironment. For instance, tumor-infiltrating lymphocytes (TILs) are enriched in certain GBM subtypes and depleted in others.10 IDH-WT tumors are also associated with higher TIL infiltration.10 IDH mutational status and GBM transcriptional subtypes also affect the presence of macrophages, neutrophils, and other immune cells within the tumor microenvironment.10 Mimicking this additional layer of heterogeneity presents a further challenge for traditional preclinical models.
On a more macro level, in vitro and most in vivo models fail to mimic the blood-brain barrier (BBB), a major reason why promising drug candidates for GBM have failed.11 Crossing the BBB is a huge challenge for drug development across many CNS indications and 98% of small molecules and 100% of large-molecule therapeutics fail to accumulate at therapeutically relevant concentrations.11
The Path Forward: More Accurate In Vivo Glioblastoma Mouse Models
While in vitro models are a mainstay in preclinical drug screening, for GBM, reliable and clinically accurate in vivo models are a necessary complement to drive drug discovery and development forward. As it stands today, there are three major in vivo GBM mouse models used, with their own sets of advantages and disadvantages.
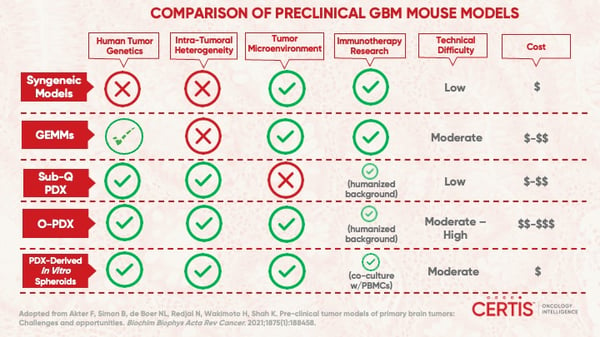
Syngeneic Mouse Models
Several syngeneic GBM tumor models have been developed through the induction of GBM tumors using alkylating agents, such as ENU or other mutagens. Many syngeneic models use rats and cell lines with mutations in Braf, Tp53, Pdgfra, Cdkn2a, and Egfr. In mice, syngeneic cell lines, such as GL261 and CT-2A, have been isolated and exhibit some morphological similarity to GBM.5
Advantages4,5
- Immunocompetence and immune cell-tumor interaction
- Enables testing of immunotherapeutics
- High engraftment rate
Disadvantages4,5
- Genetic drift due to passaging
- Lack of intra-tumoral heterogeneity and clinical progression
- No parenchyma infiltration
Additional advantages of these models include their relatively low cost and ease of use; however, the disadvantages have led to these models falling out of favor due to their inability to mimic human GBM heterogeneity at the morphological and molecular level.3
Genetically Engineered Models
With an increase in the utility of genetic engineering tools, genetically engineered models (GEMs) for GBM have enabled the careful study of individual genes, their temporal expression, and cell types in pathogenesis and treatment resistance.5 Various methods including virus-based, Cre-LoxP, and transposon-based techniques have been developed and used to introduce, overexpress, or suppress oncogenic genes in specific cells.
Advantages4,5
- Immunocompetence and immune cell-tumor interaction
- Enables testing of immunotherapeutics
- Recapitulation of human tumor genetics through precise engineering
Disadvantages4,5
- Development from scratch is time-consuming and costly
- Homogenous genetic changes in GBM tumor
- Tumor biology affected by the genetic background of mice
Several sophisticated studies have been conducted using GBM GEMs. Chen et al. developed a useful model for tracking the proliferation of GSCs and used it to study GBM recurrence following temozolomide discontinuation.12 Another notable example was the creation of a Cre-LoxP mouse model capable of expressing with WT and/or vIII human EGFR by Zhu et al.5,13 Expression is controlled through injection of Cre recombinase, resulting in the formation of aggressive GBM tumors with high penetrance in six to eight weeks.5,13
Orthotopic Patient-Derived Xenografts (O-PDX)
The major disadvantage of syngeneic models and GEMs is that they fail to account for the genetic, transcriptomic, and spatial heterogeneity that human GBM tumors exhibit in the clinic. By contrast, using patient-derived xenograft (PDX) models allow the implantation of real human tumors into immunodeficient mouse models for preclinical efficacy screening.
There has been significant debate within the PDX community about whether subcutaneous or orthotopic methodologies better mimic the relevant clinical characteristics of different types of cancer. While subcutaneous PDX techniques are more technically feasible for tracking tumor growth and treatment response, they do not accurately mimic the tumor microenvironment or the presence of the BBB.
It is now well-accepted that implantation intracranially, at an orthotopic site, provides a model that best recapitulates many of the clinical characteristics of GBM, while accounting for the inter- and intra-tumoral heterogeneity of GBM.4,5 Moreover, O-PDX models developed by Joo et al. show that tumors retain the same genomic, histological, epigenetic, and treatment response characteristics as parental tumors.4,14 In addition, O-PDX models exhibit high engraftment rates (~75%), though this doesn’t apply to all O-PDX models.5,14 In general, engraftment rate and length of engraftment are affected by the origin and aggressiveness of a tumor.5 In some cases, passaging tumors in vitro, as organoids or neurospheres or in vivo, as a subcutaneous PDX, can enable higher success rates, but this can also lead to a loss of the tumor microenvironment and divergence from the genomic features of the parental tumor4,15
Advantages4,5
- Recapitulates the patient’s tumor genetics and heterogeneity
- Most clinically-relevant phenotypes
- Accommodates cell-, organoid-, and neurosphere-based xenografting
Disadvantages4,5
- Success rates are variable depending on the patient-derived tumor
- Technically difficult and costly
- Lack immune cells and ability to test immunotherapies
Next Steps in GBM Drug Discovery: The Need for Well-Characterized O-PDX Models
The inability to develop drugs that significantly improve survival rates in GBM patients highlights the compelling need to revisit current preclinical study designs and prioritize the use of clinically relevant preclinical GBM models and intracranial engraftment techniques that take the blood brain barrier (BBB) and intratumoral heterogeneity into account. Certis Oncology Solutions is dedicated to helping drug developers fulfill the unmet need for safe and efficacious GBM therapeutics.
Developing a well-characterized bank of patient-derived GBM models that captures the breadth of heterogeneity present in the clinic is a necessary first step to drive widespread O-PDX adoption in GBM drug development.
Learn more about how Certis is advancing GBM drug development through well-characterized orthotopic patient-derived xenograft (O-PDX) models that closely recapitulate the clinical characteristics of GBM and account for inter- and intra-tumoral heterogeneity4,5 as well as specialized intracranial engraftment and dosing techniques.
Now Enrolling: Glioblastoma In Vitro CertiScreen™
Searching for a quick and cost-effective way to evaluate the preclinical efficacy and mechanisms of action (MOA) of your glioblastoma (GBM) candidates? This screen includes up to nine well-characterized orthotopic intracranial GBM 3D spheroid models, with patient history, treatment history; survival rates, growth kinetics, growth sensitivity to temozolomide (TMZ), and stem cell marker data.

Learn more about this time-sensative screen.
References
1 National Brain Tumor Society. Quick Brain Tumor Facts. Accessed on: Aug. 4, 2022.
2 National Brain Tumor Society. Glioblastoma Facts & Figures. Accessed on: Aug. 4, 2022.
3 Fernandes C, Costa A, Osório L et al. Current Standards of Care in Glioblastoma Therapy. In: De Vleeschouwer S, editor. Glioblastoma [Internet]. Brisbane (AU): Codon Publications; 2017 Sep 27. Ch 11. NIH website.
4 Patrizii M, Bartucci M, Pine SR, Sabaawy HE. Utility of Glioblastoma Patient-Derived Orthotopic Xenografts in Drug Discovery and Personalized Therapy. Front Oncol. 2018;8:23. Published 2018 Feb 12.
5 Akter F, Simon B, et al. Preclinical Tumor Models of Primary Brain Tumors: Challenges and Opportunities. Biochim Biophys Acta Rev Cancer. 2021;1875(1):188458.
6 Sottoriva A, Spiteri I, Piccirillo SG et al. Intratumor Heterogeneity in Human Glioblastoma Reflects Cancer Evolutionary Dynamics. Proc Natl Acad Sci U S A. 2013;110(10):4009-4014.
7 Verhaak RG, Hoadley KA, Purdom E, et al. Integrated Genomic Analysis Identifies Clinically Relevant Subtypes of Glioblastoma Characterized by Abnormalities in PDGFRA, IDH1, EGFR, and NF1. Cancer Cell. 2010;17(1):98-110.
8 Qazi MA, Vora P, Venugopal C et al. Intratumoral Heterogeneity: Pathways to Treatment Resistance and Relapse in Human Glioblastoma. Ann Oncol. 2017;28(7):1448-1456.
9 Patel AP, Tirosh I, Trombetta JJ et al. Single-Cell RNA-Seq Highlights Intratumoral Heterogeneity in Primary Glioblastoma. Science. 2014;344(6190):1396-1401.
10 Pombo Antunes AR et al. Understanding the Glioblastoma Immune Microenvironment as Basis for the Development of New Immunotherapeutic Strategies. Elife. Feb. 4, 2020;9:e52176.
11 Pardridge WM. The Blood-Brain Barrier: Bottleneck in Brain Drug Development. NeuroRx. 2005;2(1):3-14.
12 Chen J, Li Y, Yu TS, et al. A Restricted Cell Population Propagates Glioblastoma Growth After Chemotherapy. Nature. 2012;488(7412):522-6.
13 Zhu H, Acquaviva J, Ramachandran P, et al. Oncogenic EGFR Signaling Cooperates With Loss of Tumor Suppressor Gene Functions in Gliomagenesis. Proc Natl Acad Sci USA. 2009;106(8):2712-2716.
14 Joo KM, Kim J, Jin J, et al. Patient-Specific Orthotopic Glioblastoma Xenograft Models Recapitulate the Histopathology and Biology of Human Glioblastomas In Situ. Cell Rep. 2013;3(1):260-273.
15 Ben-David U, Ha G, Tseng YY et al. Patient-Derived Xenografts Undergo Mouse-Specific Tumor Evolution. Nat Genet. 2017;49(11):1567-1575.
About the Author
Elie Diner has a PhD in bioengineering and 12 years of research experience in microbiology, synthetic biology and immunology. During his time at the bench, he developed a passion for effective science communication and eventually transitioned into a career as a professional science and content writer. He's authored 12 peer-reviewed scientific publications and numerous blogs, whitepapers, and eBooks for life science companies.
Back to Feed
